|
Case Report
Corneal melt in a patient with rheumatoid arthritis on methotrexate and tofacitinib
1 Department of Ophthalmology, Howard University School of Medicine, Washington, DC, USA
2 Department of Ophthalmology and Visual Sciences, University of Maryland School of Medicine, Baltimore, MD, USA
3 Department of Pathology, University of Maryland School of Medicine, Baltimore, MD, USA
4 Department of Internal Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
Address correspondence to:
Miriam B Michael
Department of Internal Medicine, University of Maryland School of Medicine, Baltimore, MD,
USA
Message to Corresponding Author
Article ID: 100007O02NN2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Nguyen NS, Lai WC, Ling C, Brown D, Rajpal S, Markidan J, Michael MB. Corneal melt in a patient with rheumatoid arthritis on methotrexate and tofacitinib. Edorium J Ophthalmol 2022;5(2):5–10.ABSTRACT
Introduction: Peripheral ulcerative keratitis (PUK) is a rare finding with a severely destructive ophthalmological emergency that typically manifests in patients with a chronic history of untreated or uncontrolled autoimmune diseases, with the most common being rheumatoid arthritis (RA).
Case Report: We present a rare case of a patient with well-controlled rheumatoid arthritis without flares for many years on methotrexate and tofacitinib who presented with rapidly progressing loss of vision and pain in the right eye due to corneal melt. She was found to have a right perforated cornea secondary to corneal melt from peripheral ulcerative keratitis (PUK) with pathology showing active inflammation. She was evaluated by the Ophthalmology and Rheumatology teams and was started on topical steroid and antibiotic eye drops alongside oral prednisone 40 mg daily. She then underwent a penetrating keratoplasty two days later. On postoperative follow-up visits, her visual acuity and ophthalmic exam remained stable with an intact graft. In patients with a longstanding history of autoimmune diseases presenting with rapid progression of eye pain, vision loss, and/or other ocular symptoms, urgent ophthalmic and rheumatologic evaluations and aggressive management with systemic immunosuppression and/or surgery are indicated to prevent poor ophthalmic outcomes and a high mortality rate.
Conclusion: Corneal melt should be considered in a patient with autoimmune diseases who presents with eye symptoms. Peripheral ulcerative keratitis should be recognized and treated early and aggressively to avoid severe complication.
Keywords: Corneal melt, Peripheral ulcerative keratitis, Rheumatoid arthritis, Tofacitinib
INTRODUCTION
Peripheral ulcerative keratitis (PUK) is a rare finding with an incidence of 3 cases per million persons/year [1]. This disease causes inflammation in the corneal limbus associated with systemic and autoimmune diseases, with the most common cause being rheumatoid arthritis. Initial studies have reported that PUK may be the initial manifestation of collagen vascular disease in up to 50% of all cases [2]. The hallmark examination findings are a corneal epithelial defect with the destruction of the peripheral corneal stroma [3]. The peripheral cornea is most implicated in PUK as it is well vascularized and its capillary network allows the deposition of circulating immune complexes [4],[5]. The extracellular stroma of the cornea is made up of glycosaminoglycans, which create a framework for embedding highly organized collagen fibrils lamellae [4],[5]. In the corneal matrix, macrophages and fibrocytes display human leukocyte antigen DR (HLA-DR) to generate local inflammatory mediators and/or aid direct antigenic stimulation. The consequences of PUK can vary from ocular pain, irritation, redness, light sensitivity, and corneal haziness to corneal melt progressive corneal stromal dissolution leading to corneal perforation and most severely, vision loss [5],[6]. Despite the advances in corneal transplantation and rehabilitation, once the process of corneal melting has begun, it is challenging to reverse and usually requires systemic immune-modulating therapy [6],[7].
CASE REPORT
We report the case of a 71-year-old female who presented to the emergency department with subacute worsening pain and decreased vision in the right eye for one month. These ocular symptoms acutely worsened over a few days prior to presentation to an intense stabbing eye pain and significantly decreased vision to where she was only able to see shadows. The patient has a past medical history of rheumatoid arthritis (RA) which was well controlled on methotrexate 10 mg weekly and tofacitinib 11 mg daily. Prior to her presentation, she did not have any flares for six years with the last flare presenting with synovitis in her right shoulder after tapering her methotrexate from 20 mg weekly to 10 mg for worsening alopecia. Tofacitinib 11 mg daily was added and she did not have any active disease since then. Prior to this flare, her last flare-up was 16 years ago and was due to insurance issues that prevented her from receiving her medicines. During this time, she was consistently seeing her ophthalmologist and her dry eyes were well controlled on Restasis twice daily with consistent visual acuity in both eyes ranging between 20/20 and 20/25. Her last examination was one year ago in which her visual acuity was 20/20 in the right eye and 20/25 in the left eye, a Schirmer test was done which was stable to prior tests indicating severe dryness with 3 mm in the right eye and 2 mm in the left eye.
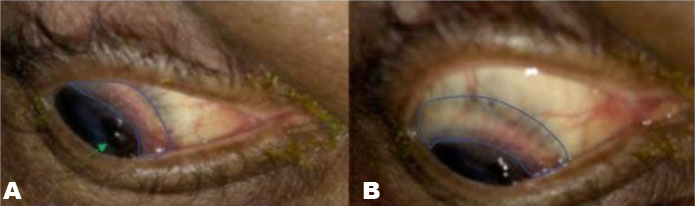
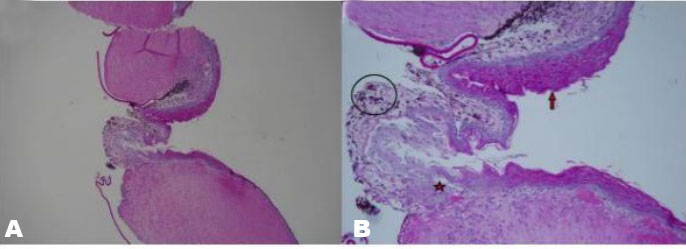
On admission to the hospital, her white blood cell (WBC) count was 2.3, platelet levels were 491. Comprehensive metabolic panels and serum electrolytes were within normal limits and glomerular filtration rate (GFR) was 48. Ophthalmology was consulted and on examination, a large 6×2 mm corneal defect with iris plugging from 1–4 clock hours was noted, accompanied by an adjacent area of scleral thinning and vascularization along the corneal limbus (Figure 1A and Figure 1B). B-scan ultrasonography confirmed the retina to be attached without signs of vitritis. She was diagnosed with a corneal melt secondary to PUK in the right eye and was started on topical prednisolone acetate every 2 hours and moxifloxacin eye drops 4 times daily in addition to eye protection. Two days later, she underwent a corneal transplant of the right eye with penetrating keratoplasty. Pathology report of the right host cornea described a corneal ulcer with associated hyperkeratosis, hemosiderin deposition with acute and chronic inflammation. At the site of rupture, there existed adherent pigment uveal cells, full-thickness inflammation, destruction of both Bowman’s, and Descemet’s membrane (Figure 2A and Figure 2B).
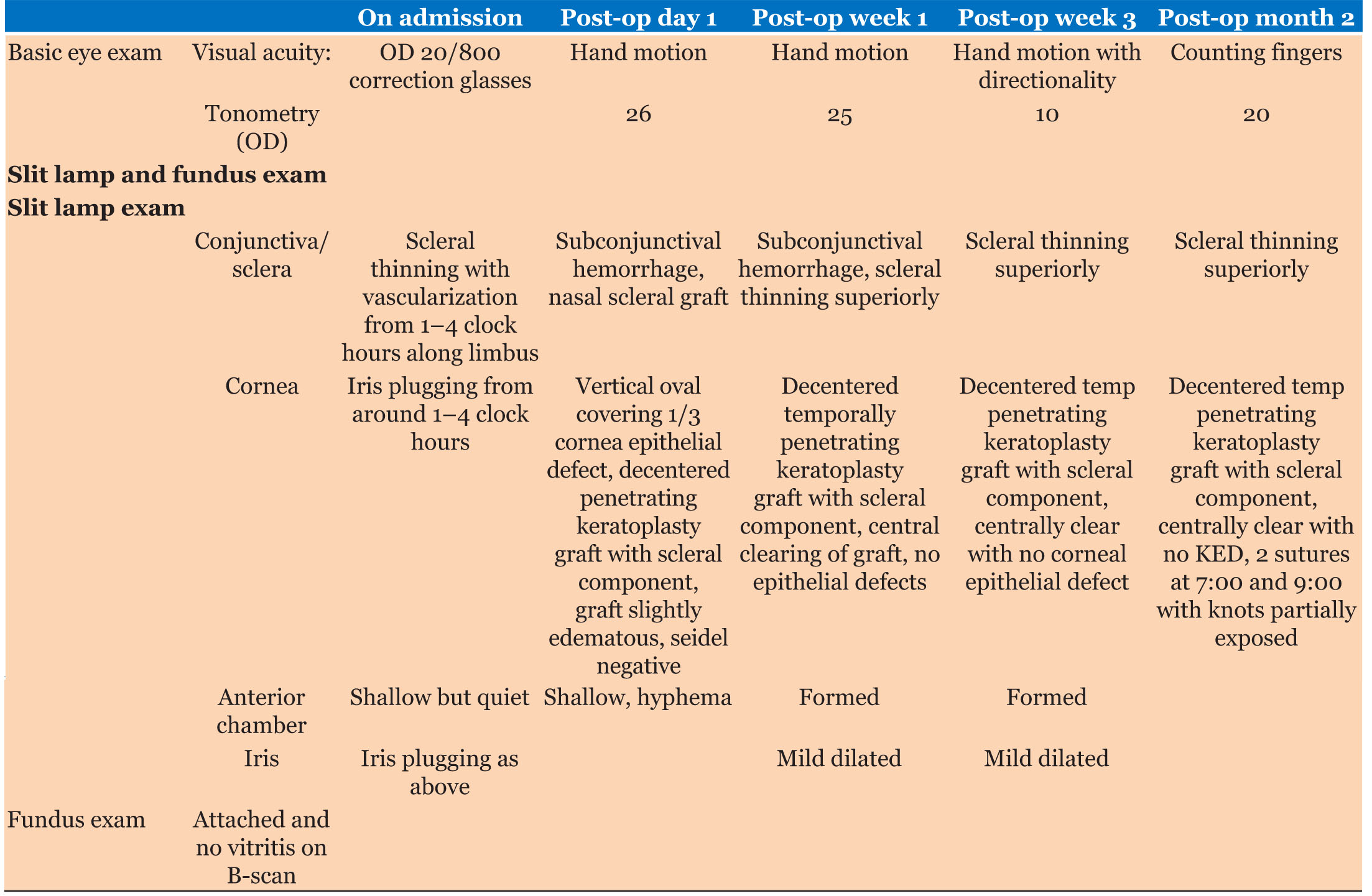
On postoperative day 1, her visual acuity was hand motion (HM) without directionality and intraocular pressure (IOP) was 26 mmHg. The corneal graft was slightly decentered with an overlying epithelial defect, but no leakage was noted from the graft. Rheumatology was consulted and the team diagnosed the corneal perforation associated with a flair in her rheumatoid arthritis and recommended the patient continue on methotrexate 2.5 mg once a week, folic acid 1 mg daily, tofacitinib 11 mg daily, and to start the patient on oral prednisone 40 mg daily with a plan for tapering on follow-up. At the postoperative week 1 visit, her visual acuity and intraocular pressure remained stable, and the graft was intact with the resolution of the epithelial defect and clearing of the cornea centrally. At her postoperative week 3 visit, visual acuity improved to hand motion with directionality, and IOP decreased to 10 mmHg in the right eye; the rest of the visual exam remained stable. Postoperative month 2 visit, the patient had improved vision to Count Fingers, and graft showed no signs of rejection (Figure 3, Table 1). She followed up with her rheumatologist 1 month after her surgery, there were no active joint findings, but given the corneal perforation, her methotrexate was increased to 20 mg per week and she has tapered to prednisone 5 mg daily.
DISCUSSION
The most destructive and severe ophthalmological manifestation of autoimmune disease is peripheral ulcerative keratitis (PUK), which has been reported in around 15–25% of patients with RA [3]. Approximately half of all noninfectious PUK cases are associated with collagen vascular diseases, including RA, systemic lupus erythematosus (SLE), microscopic polyangiitis, eosinophilic granulomatosis with polyangiitis, granulomatosis with polyangiitis, and/or polyarteritis nodosa. Of these disorders, RA is the most common, accounting for 34% of noninfectious PUK cases [7]. These systemic autoimmune diseases, especially if untreated, are associated with a poor prognosis for the eye and may contribute to a high mortality rate [8]. In addition, PUK can develop as a sequela of necrotizing scleritis, which is a severe, destructive vasculitic disease associated with RA that can significantly increase the mortality rate [2].
The differential diagnosis, when presented with a patient suspected of PUK, includes HIV/AIDs and numerous bacterial, fungal, and parasitic infectious etiologies thus management requires corneal or conjunctival scraping and cultures to exclude infectious etiologies before initiating anti-inflammatory medications [9]. Mooren’s ulcer, an idiopathic progressive peripheral corneal thinning and superficial vascularization that is not associated with scleritis and develops in the absence of any systemic disease must be excluded. The main difference from PUK is the lack of associated systemic findings, the severity of pain, which is more intolerable in Mooren’s ulcer and does not involve the sclera [7],[8]
The main therapy for RA-associated PUK is focused on aggressively controlling the ocular surface inflammation with a combination of topical and systemic steroids, immunosuppressive agents, and occasionally non-steroidal anti-inflammatory drugs (NSAIDs). However, NSAIDs and steroids may potentiate further ulceration and perforation [10]. This risk must be weighed with the documented benefits as pulsed intravenous immunosuppressive doses of methylprednisolone have been shown to stop the progression of PUK in these patients [11]. Methotrexate is the most efficacious in most patients. Secondary agents with higher potential toxicity, such as cyclophosphamide, azathioprine, and cyclosporine, are reserved for selected cases with drug intolerance and rapidly progressive disease. In addition to immunotherapy, lubricating agents are advised to promote the healing of the epithelium [12]. Other ocular surface management can be considered such as amniotic membrane grafts or tarsorrhaphy.
Tofacitinib is a new drug used for patients with moderate to severe RA. Tofacitinib is a recently approved synthetic targeted disease-modifying agent which can be used as a monotherapy or combined with other disease modifying agents [13]. It has been shown to have a significant effect on the treatment of various vasculitic disorders and has been successful in the treatment of refractory uveitis and scleritis [14], which makes the rapid decline and clinical course in this patient developing corneal melt on this agent noteworthy.
Although PUK typically manifests in patients with a long history of untreated or uncontrolled rheumatoid arthritis, it can occasionally be the initial presentation in patients with RA. We report a rare case of a patient with long-standing RA well controlled on methotrexate and tofacitinib without any systemic or musculoskeletal flares reported in six years. Our patient did have severe chronic keratoconjunctivitis sicca (KCS) consistent with her history of RA, which leads to lacrimal gland destruction and ocular surface inflammation [15]. While it is possible that the keratoconjunctivitis sicca could have contributed to the development of PUK, this is less likely given the patient’s stable ocular examinations and well-controlled symptoms on Restasis with objective stability in the Schirmer test. The authors believe it is likely that this presentation was an acute flare-up of her rheumatoid arthritis.
Peripheral ulcerative keratitis can lead to serious ocular complications, with the corneal ulcer sometimes rapidly progressing to corneal melt syndrome (keratolysis), and up to 30% of those patients getting ocular perforation within days. Half of the patients may require urgent corneal or anterior segment surgery. However, surgery alone cannot control the underlying inflammatory process and is inadequate to prevent recurrences. As such, these are palliative and temporizing options. Although the integrity of the globe can be maintained with the combination of surgery and immunotherapy, the visual outcome remains insignificant. The use of tissue adhesive or corneal glue with a bandage contact lens also can help delay the need for corneal surgery and facilitate definite healing in some cases [8],[12].
CONCLUSION
Peripheral ulcerative keratitis (PUK) is a destructive and severe ophthalmological manifestation of autoimmune disease. Although our patient presented without a systemic flare in several years on methotrexate and tofacitinib, her presentation and rapid progression to corneal melt represented an acute flare in her disease process. This is important to recognize and aggressively manage with systemic immunosuppression, as untreated symptoms are associated with a poor prognosis for the eye and may contribute to a high mortality rate.
REFERENCE
1.
McKibbin M, Isaacs JD, Morrell AJ. Incidence of corneal melting in association with systemic disease in the Yorkshire Region, 1995–7. Br J Ophthalmol 1999;83(8):941–3. [CrossRef]
[Pubmed]

2.
Tauber J, Sainz de la Maza M, Hoang-Xuan T, Foster CS. An analysis of therapeutic decision making regarding immunosuppressive chemotherapy for peripheral ulcerative keratitis. Cornea 1990;9(1):66–73.
[Pubmed]

3.
Cao Y, Zhang W, Wu J, Zhang H, Zhou H. Peripheral ulcerative keratitis associated with autoimmune disease: Pathogenesis and treatment. J Ophthalmol 2017;2017:7298026. [CrossRef]
[Pubmed]

4.
Watanabe R, Ishii T, Yoshida M, et al. Ulcerative keratitis in patients with rheumatoid arthritis in the modern biologic era: A series of eight cases and literature review. Int J Rheum Dis 2017;20(2):225–30. [CrossRef]
[Pubmed]

5.
Silva BL, Cardozo JB, Marback P, Machado FC, Galvão V, Santiago MB. Peripheral ulcerative keratitis: A serious complication of rheumatoid arthritis. Rheumatol Int 2010;30(9):1267–8. [CrossRef]
[Pubmed]

6.
7.
Yagci A. Update on peripheral ulcerative keratitis. Clin Ophthalmol 2012;6:747–54. [CrossRef]
[Pubmed]

8.
Messmer EM, Foster CS. Vasculitic peripheral ulcerative keratitis. Surv Ophthalmol 1999;43(5):379–96. [CrossRef]
[Pubmed]

9.
Lin YY, Jean YH, Lee HP, et al. Excavatolide B attenuates rheumatoid arthritis through the inhibition of osteoclastogenesis. Mar Drugs 2017;15(1):9. [CrossRef]
[Pubmed]

10.
Jayson MI, Jones DE. Scleritis and rheumatoid arthritis. Ann Rheum Dis 1971;30(4):343–7. [CrossRef]
[Pubmed]

11.
Messmer EM, Foster CS. Destructive corneal and scleral disease associated with rheumatoid arthritis. Medical and surgical management. Cornea 1995;14(4):408–17. [CrossRef]
[Pubmed]

12.
Bernauer W, Ficker LA, Watson PG, Dart JK. The management of corneal perforations associated with rheumatoid arthritis. An analysis of 32 eyes. Ophthalmology 1995;102(9):1325–37. [CrossRef]
[Pubmed]

13.
Kucharz EJ, Stajszczyk M, Kotulska-Kucharz A, et al. Tofacitinib in the treatment of patients with rheumatoid arthritis: Position statement of experts of the Polish Society for Rheumatology. Reumatologia 2018;56(4):203–11. [CrossRef]
[Pubmed]

14.
Paley MA, Karacal H, Rao PK, Margolis TP, Miner JJ. Tofacitinib for refractory uveitis and scleritis. Am J Ophthalmol Case Rep 2019;13:53–5. [CrossRef]
[Pubmed]

15.
Kang MH, Kim MK, Lee HJ, Lee HI, Wee WR, Lee JH. Interleukin-17 in various ocular surface inflammatory diseases. J Korean Med Sci 2011;26(7):938–44. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgement
There are no significant parties that have contributed to the case report that have not been acknowledged as a patient, writer, or reference.
Author ContributionsNguyen Sy Nguyen - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Wei Chen Lai - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Carlthan Ling - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Douglas Brown - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sachin Rajpal - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Janina Markidan - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Miriam B Michael - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Nguyen Sy Nguyen et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.