|
Short Report
Two double flanged versus four flanged in scleral fixated IOL: A descriptive study
1 Ophthalmology Department, RSUD Tenriawaru Hospital, Bone, South Sulawesi, Indonesia
2 Cerebellum Clinic, Makassar, South Sulawesi, Indonesia
Address correspondence to:
George Ade Sitanaya
Jl. Sungai Walanae no. 2, Makassar, Sulawesi Selatan,
Indonesia
Message to Corresponding Author
Article ID: 100004O02GS2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Sitanaya GA, Phoaniary R, Ibrahim DF. Two double flanged versus four flanged in scleral fixated IOL: A descriptive study. Edorium J Ophthalmol 2020;3:100004O02GS2020.ABSTRACT
Aims: To describe a new method for scleral fixated intraocular lens (IOL) and to report its long-term follow-up. This study also shows the comparison of the new method with the current popular method that is four flanged scleral fixated IOL.
Method: Six patients who underwent the new method (two double flanged IOL) and 6 patients underwent four flanged scleral fixated IOL. Postoperative data was collected and recorded, such as visual acuity, intraocular pressure, anterior chamber activity, sign of IOL decentration/tilting and subjective complaints from the patients. Follow-up was done for 4–8 weeks.
Result: Among the first group (two double flanged IOL) the mean visual acuity are 0.28 and 0.34 [uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA)]. The second group (four flanged IOL) the mean visual acuity are 0.29 and 0.35 (UCVA and BCVA). There is no (0%) IOL decentration of both the groups during the follow-up period. No significant anterior chamber reaction was found in both groups.
Conclusion: The two double flanged IOL can be used as alternative method for intrascleral IOL fixation. It provides good long-term stabilization, no need for specific IOL, or any hard to obtain material.
Keywords: Aphakia, Dislocation, Intrascleral IOL, Secondary IOL, Subluxation
INTRODUCTION
Cataract surgery and intraocular lens (IOL) implantation is the most performed operation in the field of ophthalmology. However, sometimes IOL cannot be planted in its physiological position (in the bag). Therefore, several secondary IOL fixation techniques have been done [1],[2],[3],[4],[5],[6].
Scleral fixation and iris fixation were the most widely used techniques of the present era. Although popular, the technique of iris fixation has some disadvantages, such as: distorted pupil, which can make it difficult to evaluate the posterior segment due to undilated pupil, more inflammatory reactions, less stable visual acuity, and refraction. For these reasons, scleral fixation techniques remain the main choice in the secondary IOL implantation technique [1],[2],[3],[4],[5],[6].
Traditional scleral fixation technique used 10.0 sutures, tied into the haptics, or the IOL eyelet and then passed into the sclera/Hoffman pocket. This method is not popular anymore due to long and difficult process (surgery) and its long-term instability of the IOL due to suture breakdown that leads to decentered IOL [2].
Yamane technique was a fairly popular technique in the new era of scleral fixation. It is quite fast of a procedure in the right hand/surgeon, no suture problem, and has good long-term stability. However, Yamane technique also has limitations, which are: the need of a special IOL that is not easily available (IOL used should be a 3-piece IOL with strong haptic), very steep learning curve due to difficult intraocular manipulation, and less stable visual acuity due to pseudo-phacodenesis. Because of these reasons, many ophthalmologists proposed a new technique to address the drawbacks of previous technique [1].
Glued IOL technique was similar to Yamane technique but used fibrin glue to secure the haptic at the scleral pocket. The main purpose of glued IOL was to prevent pseudo-phacodenesis and to improve IOL stability, so that it would improve the visual acuity. However, the main drawback of the technique had the difficulty to obtain the fibrin glue [3].
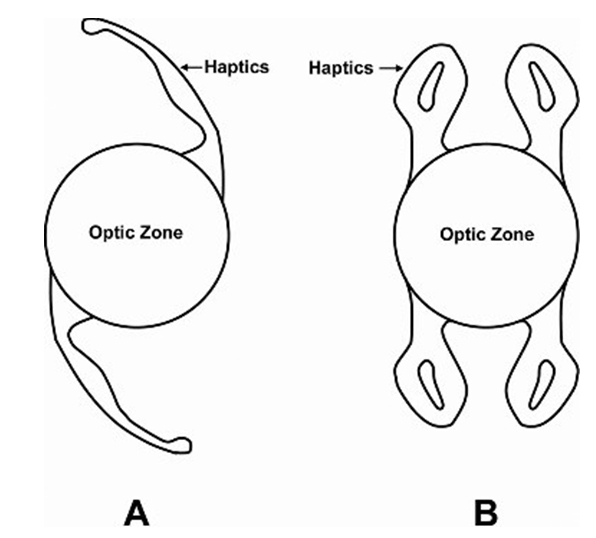
Flanged technique was one of the new methods in scleral fixation. Flanged was achieved by heating (using dry handheld cautery) the end of polypropylene material. The common way of flanged technique is by using 5.0/6.0 polypropylene suture and 4 haptic IOL/4 eyelet IOL. The polypropylene sutured was passed from sclera into each of the haptic and flanged at the suture end to prevent the slippage of the suture back into the eye. Because there are four flange totals, hence the technique commonly known as four flanged technique [1],[5].
Four flange IOL technique no doubt has several superiorities compared to other techniques. Excellent stability of the IOL due to four-point fixation and minimal intraocular manipulation were the main reasons that this technique is preferred by many. However, it has several drawbacks, such as: the need to find specific IOL, relatively larger incision, larger pupil diameter (to avoid cross wiring), and relatively difficult and longer to perform.
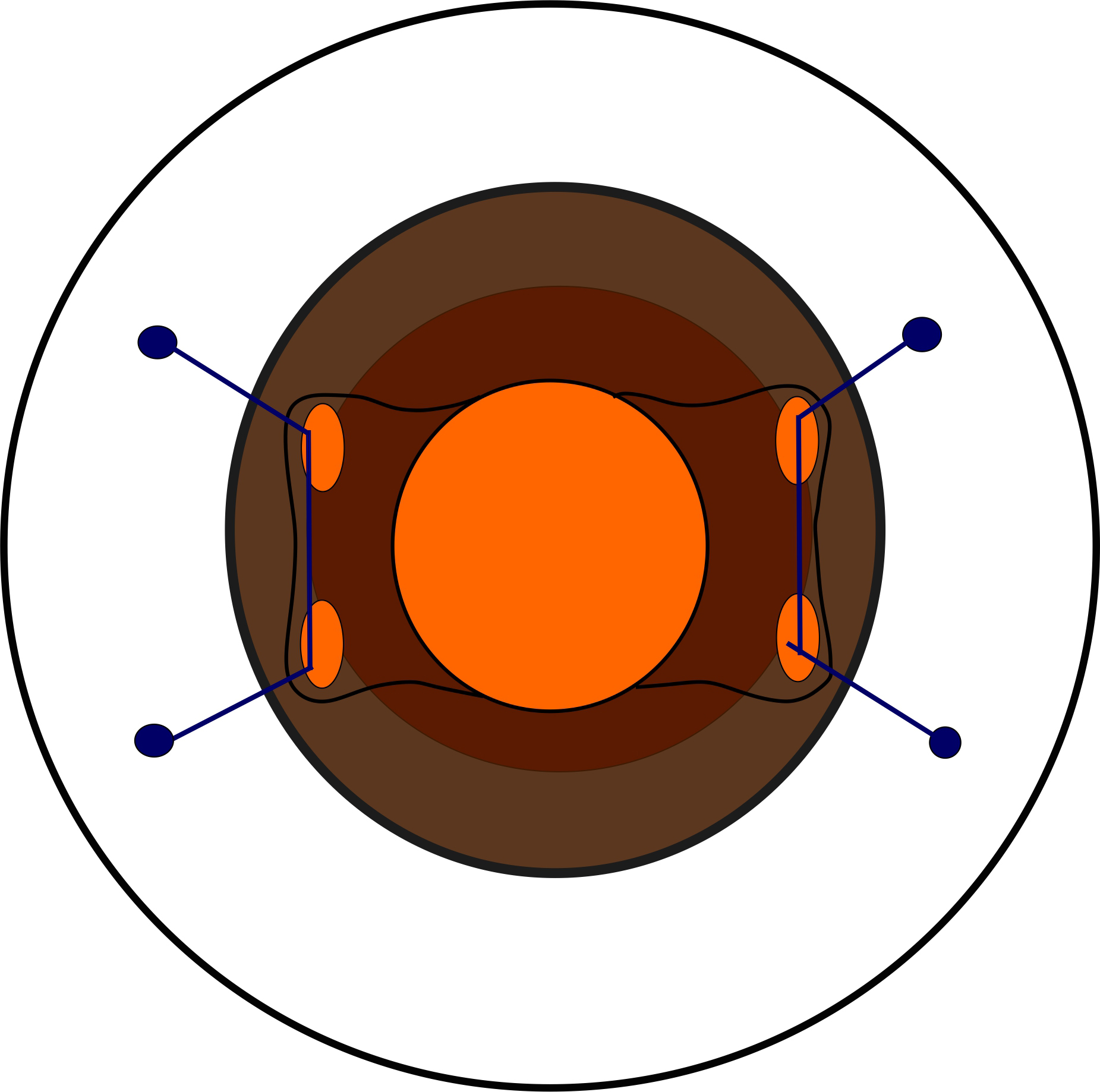
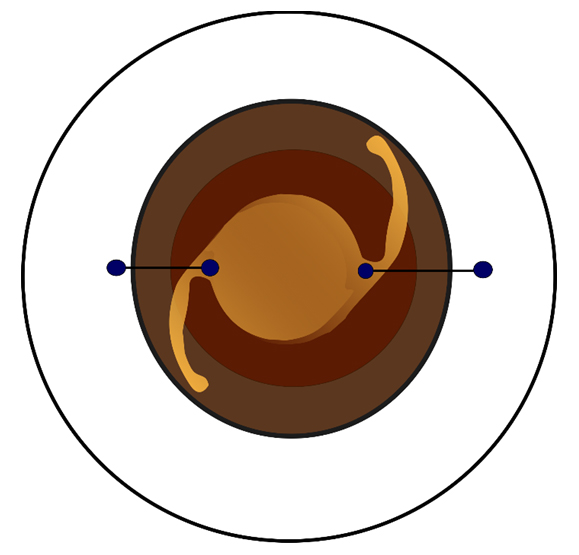
Two double flanged IOL technique was a technique that created a pseudo-haptic by passing two polypropylene sutures into the IOL and docking the suture into the sclera 180° away from each other. Both ends of the suture were flanged to prevent the slippage (Figure 1 and Figure 2).
Aims
This short report is aimed to describe a new method of scleral fixation IOL implantation and to report its long-term follow-up. Also, to compare the new method with the current popular method which is four flanged scleral fixated IOL.
METHODS
This study used prospective study. Data was collected in 12 months (January 2019–January 2020). Twelve aphakic patients were screened and assigned into two groups. All patients had similar characteristics, which are no posterior segment abnormalities, normal axial length, and good corneal clarity. Baseline uncorrected visual acuity and intraocular pressure were recorded. All patients were examined by using slit lamp for anterior segment and indirect ophthalmoscope for posterior segment evaluation. Axial length and IOL calculation were taken by using A-scan ultrasound biometry. Six patients who underwent the new method (two double flanged IOL) and 6 patients underwent four flanged scleral fixated IOL. All the surgeries were performed by one surgeon.
Postoperative data was collected and recorded, such as visual acuity, intraocular pressure, anterior chamber activity, sign of IOL decentration/tilting, and subjective complaints from the patients. Follow-up was done for 4–8 weeks. All postoperative care and record were performed by other surgeon.
Technique
Two Double Flanged IOL
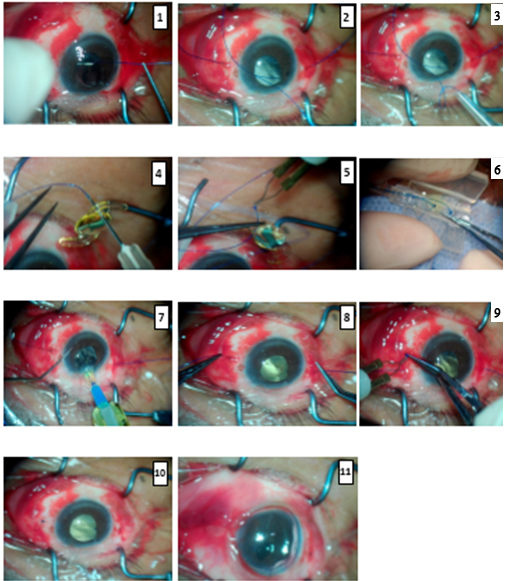
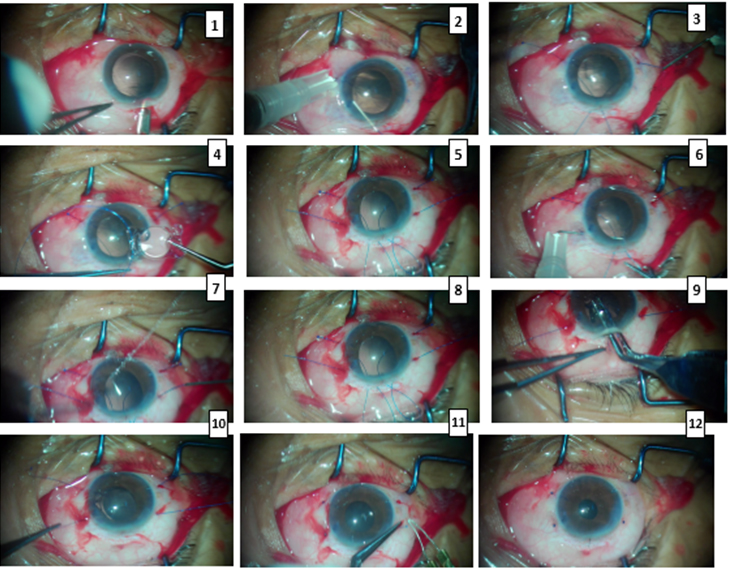
This technique was the modification of Yamane scleral fixation. After sub-tenon anesthesia, conjunctival peritomy was done in 3 o’clock and 9 o’clock direction. Anterior vitrectomy was performed to ensure there was no vitreous trapped in the anterior chamber. A 5.0 polypropylene suture was docked into the sclera, 2 mm from the limbus area, at 3 o’clock and 9 o’clock direction using 27.0 G needle. The suture was then externalized from main port at 6 o’clock then passed into the IOL cartridge. The suture then docked into the IOL using 27.0 G needle, at the optic-haptic junction then flanged at the end to secure it (Figure 3). The IOL then loaded into the cartridge as usual then delivered into the eye via 2.75 mm main port. The suture that passed from sclera was cut and flanged. The main port was secured by nylon suture, conjunctiva was closed by 8.0 polyglycolic acid (PGA) suture. Air bubble was injected into the anterior chamber to prevent vitreous prolapse and to keep anterior chamber well formed. Step-by-step surgical technique is given in Figure 4.
Four Flanged in Scleral Fixated IOL
This technique is similar to two double flanged IOL but instead using one-piece foldable IOL, it requires specific IOL which is plate haptic IOL or four haptic IOL with four holes. To prevent crosswire, each half side was done completely then moved to other half side. First, 6.0 polypropylene suture was docked at the sclera at 10 o’clock direction then externalized from the main port (5 mm scleral tunnel). This suture then went into the haptics of the IOL (one side only) then internalized again and docked at the sclera at 8 o’clock direction. Then the other side was done using the same method, the suture was docked at 2 o’clock sclera, then externalized from the main port. Then the suture went into the haptics of the IOL and internalized again and docked at the sclera at 4 o’clock. The suture was then cut short and flanged. Scleral tunnel was then sutured using 10.0 nylon suture and the rest of the technique is similar with the two double flanged IOL technique. Step-by-step surgical technique is given in Figure 5.
RESULTS
In an analysis of 12 eyes which were divided into two groups, the first group underwent two double flanged IOL procedure and the second group underwent four flanged IOL.
Intraoperative
Surgery in both groups took various amount of time (from 20 to 50 minutes). Large portion of the surgical time was spent extraocular especially in first group. Preparing the IOL was quite tricky to avoid cross wiring and it was very difficult to undo once the IOL was already inside the eye. Therefore, the sutures were docked into the IOL at the outside (extraocular) then the IOL was delivered into the eye when everything was set. The duration of the surgery also depends on the pupil size and the regularity of the pupil. Small pupil needed extra step like iris retractor insertion, while the irregular pupil needed pupilloplasty (iris suture) at the end to avoid glare and improve visual acuity.
Postoperative
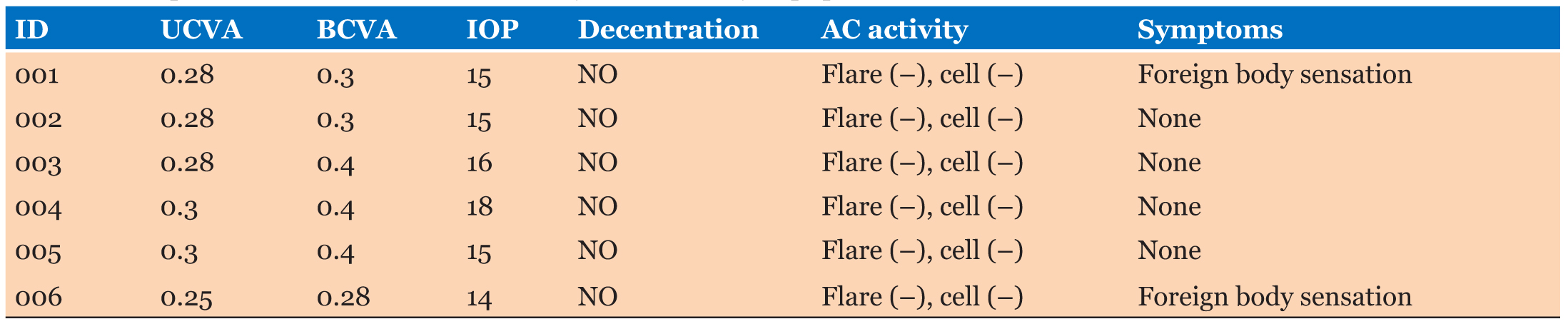
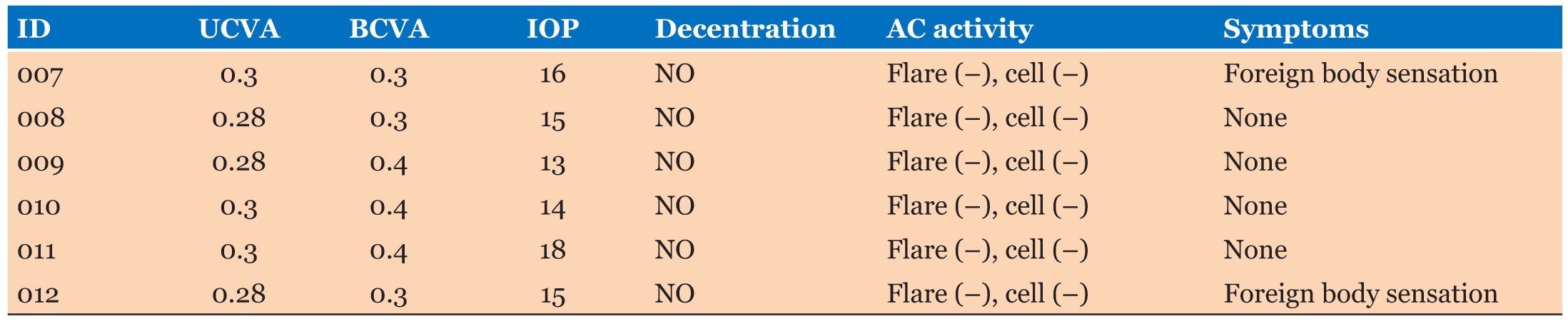
Among the first group (two double flanged IOL), the mean visual acuity are 0.28 and 0.34 (UCVA and BCVA). The second group (four flanged IOL) the mean visual acuity are 0.29 and 0.35 (UCVA and BCVA). There is no (0%) IOL decentration of both the groups during the follow-up period (4–8 weeks). Corneal edema was the main complication in postoperative, however, all resolved completely after 14th days (by the third visit). No significant anterior chamber reaction was found in both groups. Intraocular pressure in both groups was within normal limit. Posterior segment was evaluated in each visit with indirect ophthalmoscope and the results showed that there are no abnormalities in posterior segment in both the groups. Complete results are displayed in Table 1 and Table 2.
DISCUSSION
Scleral fixation IOL was the most common choice for IOL implantation when the physiological condition (in the bag IOL) cannot be done. Scleral fixation had evolved from quite complex and long surgery (due to the requirement of scleral pocket, looping, and suturing) to simpler step. Yamane et al. in his study introduced his way of making the IOL haptics flanged with the help of low temp monopolar cautery. Canabrava et al. specifically mentioned that only monofilament polypropylene suture can be flanged properly [1],[2],[3],[4] [5],[6].
Monofilament polypropylene suture has been commercially available since 1969 and has steadily gained popularity among cardiac and vascular surgeons for tissue-to-tissue suture lines as well as prosthetic-to-tissue suture lines. Advantages of polypropylene include excellent maintenance of tensile strength with no biodegradation, a low coefficient of friction giving less tissue trauma in suturing, low tissue reactivity, low thrombogenicity, less chance of infection, and some evidence of less intraoperative blood loss. The use of polypropylene suture (flanged) in ophthalmology field especially in implants is still off label; however, there are many reports that show that ophthalmologists successfully use polypropylene suture in implants like capsule tension ring (Cionni’s ring), capsule tension segments, and scleral fixation IOL [5],[8],[9],[10],[11].
In this study, we compare the results by using standard foldable IOL with 2-point fixation (the two double flanged technique) versus 4-point fixation using four haptics IOL (four flanged technique). All surgeries in this study were secondary IOL implant. All patients were aphakic from surgery done at other centers and we do not have data about previous surgery.
Postoperative results were satisfactory and similar in both the groups, even though it did not reach 1.0 visual acuity. Many factors caused the results, the most likely is a mild disturbance at the posterior segment. Even though the posterior segments were examined routinely with limited equipment (using indirect ophthalmoscope), there were maybe hidden abnormalities that were missed but can be detected by using readvance equipment [e.g., optical coherence tomography (OCT)].
Irregular astigmatism could also be the factor of the slightly sub-optimal visual acuity. All 12 patients in this study were aphakic for quite some time and underwent other procedure previously (lens extraction without IOL). All of the previous procedures used wide clear corneal incision [assume extracapsular cataract extraction (ECCE)]. This adds the amount of irregular astigmatism of the cornea.
Slight IOL tilting could also be a cause for sub-optimal visual acuity. In this study, there were no patients with IOL decentration; however, there could be a slight tilt of the IOL that can be detected with anterior OCT or anterior ultrasound bio microscopy (UBM).
There were no major postoperative complications in this study; however, this study has limitations in the follow-up term. Follow-up term only lasts from 4 to 8 weeks because most of the patients came far away from the hospital and cannot afford (economic factor) to came regularly. Other limitation was the small number of sample size.
CONCLUSION
In conclusion, two double flanged IOL technique can be used as alternative method for intrascleral IOL fixation. It provides good long-term stabilization, no need for specific IOL or any hard to obtain materials.
REFERENCE
1.
Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology 2017;124(8):1136–42. [CrossRef]
[Pubmed]

2.
Hoffman RS, Fine IH, Packer M. Scleral fixation without conjunctival dissection. J Cataract Refract Surg 2006;32(11):1907–12. [CrossRef]
[Pubmed]

3.
Agarwal A, Kumar DA, Jacob S, Baid C, Agarwal A, Srinivasan S. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg 2008;34(9):1433–8. [CrossRef]
[Pubmed]

4.
Kim KH, Kim WS. Comparison of clinical outcomes of iris fixation and scleral fixation as treatment for intraocular lens dislocation. Am J Ophthalmol 2015;160(3):463–9.e1. [CrossRef]
[Pubmed]

5.
Canedo AC, Rezende AC, Rezende PH, Canabrava S, Halabi N. Four-flanged intrascleral IOL fixation technique: Where are we? Ocular Surgery News. 2019. [Available at: https://www.healio.com/news/ophthalmology/20190730/fourflanged-intrascleral-iol-fixation-technique-where-are-we]

6.
Bellucci R, Pucci V, Morselli S, Bonomi L. Secondary implantation of angle-supported anterior chamber and scleral-fixated posterior chamber intraocular lenses. J Cataract Refract Surg 1996;22(2):247–52. [CrossRef]
[Pubmed]

7.
Tao A, Lu P, Li J, et al. High resolution OCT quantitative analysis of the space between the IOL and the posterior capsule during the early cataract postoperative period. Invest Ophthalmol Vis Sci 2013;54(10):6991–7. [CrossRef]
[Pubmed]

8.
Dean RH, Pinkerton JA, Foster JH. The use of monofilament suture in vascular surgery. Surgery 1975;78(2):165–8.
[Pubmed]

9.
Gaspar MR, Movius HJ, Rosental JJ, Bell DD, Lemire GG, Odou M. Prolene sutures are not a significant factor in anastomotic false aneurysms. The American Journal of Surgery 1983;146(2):216–9. [CrossRef]

10.
SUPPORTING INFORMATION
Author Contributions
George Ade Sitanaya - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ronald Phoaniary - Conception of the work, Design of the work, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Dian FurqaniIbrahim - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 George Ade Sitanaya et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.